Fibromyalgia is a chronic pain condition characterized by pain throughout the entire body. Although it can affect both women and men, fibromyalgia has been found to be more prevalent in women.1
As there are many symptoms of fibromyalgia beyond pain, it can be confusing and overwhelming to get your head around them. In this article, learn more about fibromyalgia symptoms in women, as well as premenopausal symptoms vs. postmenopausal symptoms, with our fibromyalgia symptoms checklist.
Prevalence of Fibromyalgia in Women
Although anyone can be diagnosed with fibromyalgia, research suggests fibromyalgia is more prevalent in women. A 2017 review found the prevalence of fibromyalgia in women to be between 2.4-6.8%.2 This study reviewed 39 different papers exploring the prevalence of fibromyalgia, concluding that all studies showed a prevalence within this range.
A more recent 2022 study found out of 11,314 cases of fibromyalgia, 90.3% of patients were women and 9.7% were men.3 This study also showed an increase in fibromyalgia in women over a 15-year period, whereas this increase was not shown in men.3
It is not exactly clear why fibromyalgia is more prevalent in women than men. However, doctors have suggested that higher rates of fibromyalgia in women could be due to the way society expects men and women to respond to pain, hormonal changes women can experience through menstruation and menopause, and differences in the way males and females react to pain.
Changes in Prevalence with Age
The prevalence of fibromyalgia has been shown to increase with age, however, it can be diagnosed at any age. The average age for someone to be diagnosed with fibromyalgia is between 35-45 years old.
Although the likelihood of being diagnosed with fibromyalgia can increase with age, there are mixed findings about the impact of these symptoms as you get older. One study found that as you age, the symptoms of fibromyalgia may impact you for a longer duration but can be less severe.4 This is thought to be because older female patients with fibromyalgia either experience less symptoms or perceive experiencing a milder form of fibromyalgia.
However, as this study was only conducted on 600 people and relied on self-reported measures (rather than objective, physical measures), there are some limitations of these findings. It’s hard to definitively conclude that your experience of symptoms will change as you get older, and more research is needed..
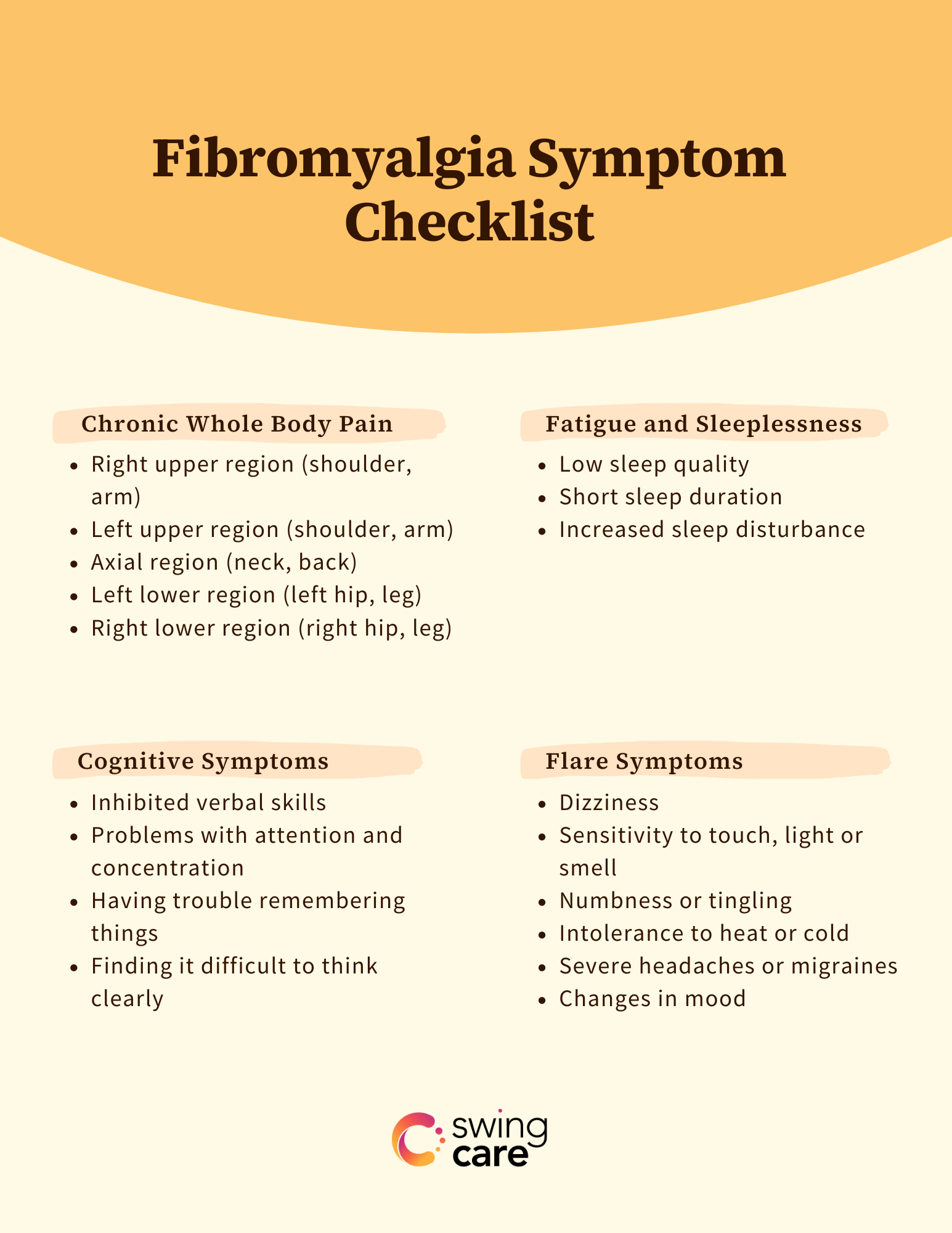
Fibromyalgia Symptom Checklist
There are a variety of symptoms of fibromyalgia in females. It can be confusing but let’s take a look at the fibromyalgia symptoms list in women.
Chronic Whole Body Pain
Widespread or whole-body pain is the trademark symptom of fibro in both females and males. Current research suggests that the way in which pain is processed in the central nervous system (CNS) is amplified in someone with fibromyalgia. This process, called central sensitization, is thought to play a key role in developing chronic pain within fibromyalgia. This involves hypersensitivity to pain within the CNS, which can lead to severe and longer-lasting pain.5
Chronic pain is classified as pain that is experienced for longer than three months, and whole-body pain must be felt in at least four out of five areas:
- Right upper region (shoulder, arm)
- Left upper region (shoulder, arm)
- Axial region (neck, back)
- Left lower region (left hip, leg)
- Right lower region (right hip, leg)
Some research suggests that pain is worse all over the body in women6 and that women can experience more widespread pain than men.3 However, this may also be affected by some of the sociological factors at play.
Fatigue and Sleeplessness
A review of multiple studies found a link between fibromyalgia and fatigue, with 76% of people with fibromyalgia reporting fatigue.7 Research has also found women with fibro experience more fatigue and greater ‘morning fatigue’ than men with fibromyalgia.8
Sleep difficulties have been found to occur frequently in individuals with fibromyalgia, including reduced sleep quality, duration, efficiency and increased sleep disturbance.9
Cognitive Symptoms
“Fibro fog,” which refers to the cognitive symptoms of fibro, include:
- Inhibited verbal skills such as slow speech
- Problems with attention and concentration
- Having trouble remembering things
- Finding it difficult to think clearly
One study found individuals with fibromyalgia had a higher frequency of cognitive symptoms compared to individuals with other pain difficulties.10 Those with fibro had more difficulties with memory, attention and language skills. This was true even after they examined the link between fibro and cognitive symptoms, whilst controlling for anxiety and depression which can both affect cognitive aspects such as memory.
Pain interference effects may help to explain these cognitive symptoms. Studies show that when pain increases, cognitive decline increases.11 This could be because pain is an attention-demanding stimulus, which uses brain areas that are also used in cognitive functions such as memory. So, if your attention is directed more to your pain, the less cognitive ability you may have to spare.
Premenopausal vs. Postmenopausal Symptoms
The impact of fibromyalgia on women has been shown to change depending on if females are experiencing menopause or not, and if they have been through menopause. In fact, those experiencing menopause are twice as likely to have chronic pain conditions like fibro. So, let’s take a look at fibromyalgia symptoms in postmenopausal women and the impact menopause can have.
Changes to Sleep and Fatigue
We already know that the research indicates sleep is affected when someone has fibromyalgia, and that there can be increased fatigue too.7.,9 During and after menopause, sleep can also be affected. The National Institute of Health reported that there can be an increase in sleep disturbance between 35%-60% post-menopause.12
Therefore, as menopause can increase the likelihood of fibromyalgia, and both fibro and menopause can have great impacts on sleep and fatigue, it’s no surprise that sleep and fatigue can be negatively impacted during this period. Although this can sound frightening or upsetting, there are a few things that may be able to help:
- Stay moving. Even when you do not have any activity planned, try to go for a walk, stretch, or keep the muscles moving in a way that’s available to you.
- Try relaxation techniques which may be able to help calm your muscles and body, such as mindfulness or breathing exercises.
- Do what you can to practice good sleep hygiene. For example, avoid caffeine and bright lights before going to bed to help give you a better chance of getting enough sleep.
If you are still unsure of what to do and are still affected by these changes in sleep and fatigue due to menopause and fibro, have a conversation with your doctor to learn about more options.
Mood Changes
Fibromyalgia can impact mood, which is completely understandable given the variety of different symptoms patients are going through. Research has found high rates of anxiety and depression in individuals with fibro and fibromyalgia has been linked with greater negative affect (which involves general distress accompanied by negative emotions such as sadness or guilt).13 This can all occur premenopause.
So, what happens postmenopause? For starters, it is common and natural for postmenopausal women to experience altered mood states such as stress, depression and anxiety which can occur due to hormonal changes. Postmenopause, these mood changes can be greater in someone with fibro because of reduced estrogen; estrogen plays a role in serotonin release, and serotonin can affect mood. Less estrogen could mean less serotonin which may result in greater mood changes postmenopause. If you couple this with other fibromyalgia symptoms such as pain, fibro fog, of course, this can make you feel more low or anxious.
This doesn’t mean that if you have fibromyalgia and have been through menopause, mood changes will be worse. This does vary from person to person and it is important to engage with self-care and things you enjoy. If your mood is affecting you significantly, consider speaking to your doctor or consulting a psychologist.
Muscle and Joint Pain
Pain in muscles and joints is common in fibromyalgia, in both men and women. However, research has shown that muscle pain is more prevalent in women postmenopause compared to premenopause.14 So, if someone is experiencing both fibro and menopause (or have been through menopause), muscle and joint pain can be worse because of the overlap in symptoms.
Take the Fibromyalgia Self-Assessment
Fibromyalgia is characterized by many different symptoms, and has been shown to be more prevalent in women. In addition, menopause has also been shown to have an impact on symptoms, due to very similar symptoms occurring in fibro and menopause and the hormone changes that can occur just before, during and after menopause.
As there are many fibromyalgia symptoms in women, it can be helpful to take your own fibromyalgia self-assessment. You can take the fibromyalgia quiz here to go through the diagnostic criteria on your own and get your score.
Medically reviewed by Dr. Andrea Chadwick, MD, MSc, FASA
Sources
- Ruschak I, Montesó-Curto P, Rosselló L, Aguilar Martín C, Sánchez-Montesó L, Toussaint L. Fibromyalgia syndrome pain in men and women: A scoping review. Healthcare (Basel). 2023 Jan 11;11(2):223. doi: 10.3390/healthcare11020223. PMID: 36673591; PMCID: PMC9859454.
- Marques AP, Santo ASE, Berssaneti AA, Matsutani LA, Yuan SLK. Prevalence of fibromyalgia: Literature review update. Revista Brasileira de Reumatologia (English Ed). 2017 Jul;57(4): 356-363. doi: 10.1016/j.rbre.2017.01.005
- Cooksey R, Choy E. Exploring gender differences, medical history and treatment in patients with fibromyalgia in the UK using primary-care data: A retrospective population-based cohort study. The Lancet Rheumatology. 2022 Sept;4(S20). doi: 10.1016/S2665-9913(22)00296-X
- Cronan TA, Serber, ER, Walen HR, Jaffe M. The influence of age on fibromyalgia symptoms. Journal of Aging and Health. 2002 Aug;14(3):370-384. doi: 10.1177/08964302014003004
- Nijs J, George SZ, Clauw DJ, Fernandez-De-Las-Penas C, Kosek E, Ickmans K, Fernandez-Carnero J, Polli A, Kapreli E, Huysmans E, Cuesta-Vargas AI, Mani R, Lundberg M, Leysen L, Rice D, Sterling M, Curatolo M. Central sensitization in chronic pain conditions: Latest discoveries and their potential for precision medicine. Lancet Rheumatol. 2021 May;3(5):E383-E392. doi:10.1016/S2665-9913(21)00032-1
- Yunus MB. The role of gender in fibromyalgia syndrome. Curr Rheumatol Rep. 2001 Apr;3(2):128-34. doi: 10.1007/s11926-001-0008-3. PMID: 11286669.
- Vincent A, Benzo RP, Whipple MO, McAllister SJ, Erwin PJ, Saligan LN. Beyond pain in fibromyalgia: Insights into the symptom of fatigue. Arthiritis Res Ther. 2013 Nov;15(221): doi: 10.1186/ar4395
- Yunus MB, Inanici F, Aldag JC, Mangold RF. Fibromyalgia in men: comparison of clinical features with women. J Rheumatol. 2000 Feb;27(2):485-90. PMID: 10685818.
- Keskindag B, Karaaziz M. The association between pain and sleep in fibromyalgia. Saudi Med J. 2017 May;38(5):465-475. doi: 10.15537/smj.2017.5.17864. PMID: 28439595; PMCID: PMC5447206.
- Rodriquez-Andreu J, Ibanez-Bosch R, Portero-Vasquez A, Masramon X, Rejas J, Galvez R. Cognitive impairment in patients with fibromyalgia syndrome assessed by the mini-mental state examination. BMC Musculoskeletal Disorders. 2009 Dec;10. doi: 10.1186/1471-2474-10-162
- Galvez-Sánchez CM, Reyes Del Paso GA, Duschek S. Cognitive Impairments in Fibromyalgia Syndrome: Associations With Positive and Negative Affect, Alexithymia, Pain Catastrophizing and Self-Esteem. Front Psychol. 2018 Mar 22;9:377. doi: 10.3389/fpsyg.2018.00377. PMID: 29623059; PMCID: PMC5874325.
- National Institutes of Health. National Institutes of Health State-of-the-Science Conference statement: management of menopause-related symptoms. Ann Intern Med. 2005 Jun 21;142(12 Pt 1):1003-13. Epub 2005 May 27. PMID: 15968015.
- Galvez-Sánchez CM, Duschek S, Reyes Del Paso GA. Psychological impact of fibromyalgia: current perspectives. Psychol Res Behav Manag. 2019 Feb 13;12:117-127. doi: 10.2147/PRBM.S178240. PMID: 30858740; PMCID: PMC6386210.
- Castro-Sanchez AM, Mataran-Penarrocha GA, Lopez-Rodriguez MM, Lara-Palomo IC, Arendt-Nielsen L, Fernandez-de-las-penas C. Gender differences in pain severity, disability, depression and widespread pressure pain sensitivity in patients with fibromyalgia syndrome without comorbid conditions. Pain Medicine. 2012 Dec;13(12): 1639-1647. doi: 10.1111/j.1526-4637.2012.01523.
