Many medical conditions are diagnosed through a diagnostic test, such as a laboratory blood test or imaging scan. These tests can often give you a definitive answer about whether or not you have been diagnosed with that specific condition. But unlike those conditions, there are no specific laboratory tests or imaging scans used to diagnose fibromyalgia. Doctors diagnose it based on symptoms and using approved diagnostic criteria, as well as ruling out other conditions that may play a part.
Widespread pain, fatigue and cognitive difficulties like brain fog are the primary indicators of fibromyalgia. But you may also have symptoms such as:
- Anxiety
- Depression
- Muscle stiffness
- Memory difficulties
- Headaches or migraines
- Difficulty thinking or concentrating
It should be noted that these symptoms can apply to many different diseases and medical conditions. Because of this, diagnosing fibromyalgia definitively is a two-part process: assessing symptoms, and ruling out these other conditions. [2]
Fibromyalgia Diagnostic Criteria
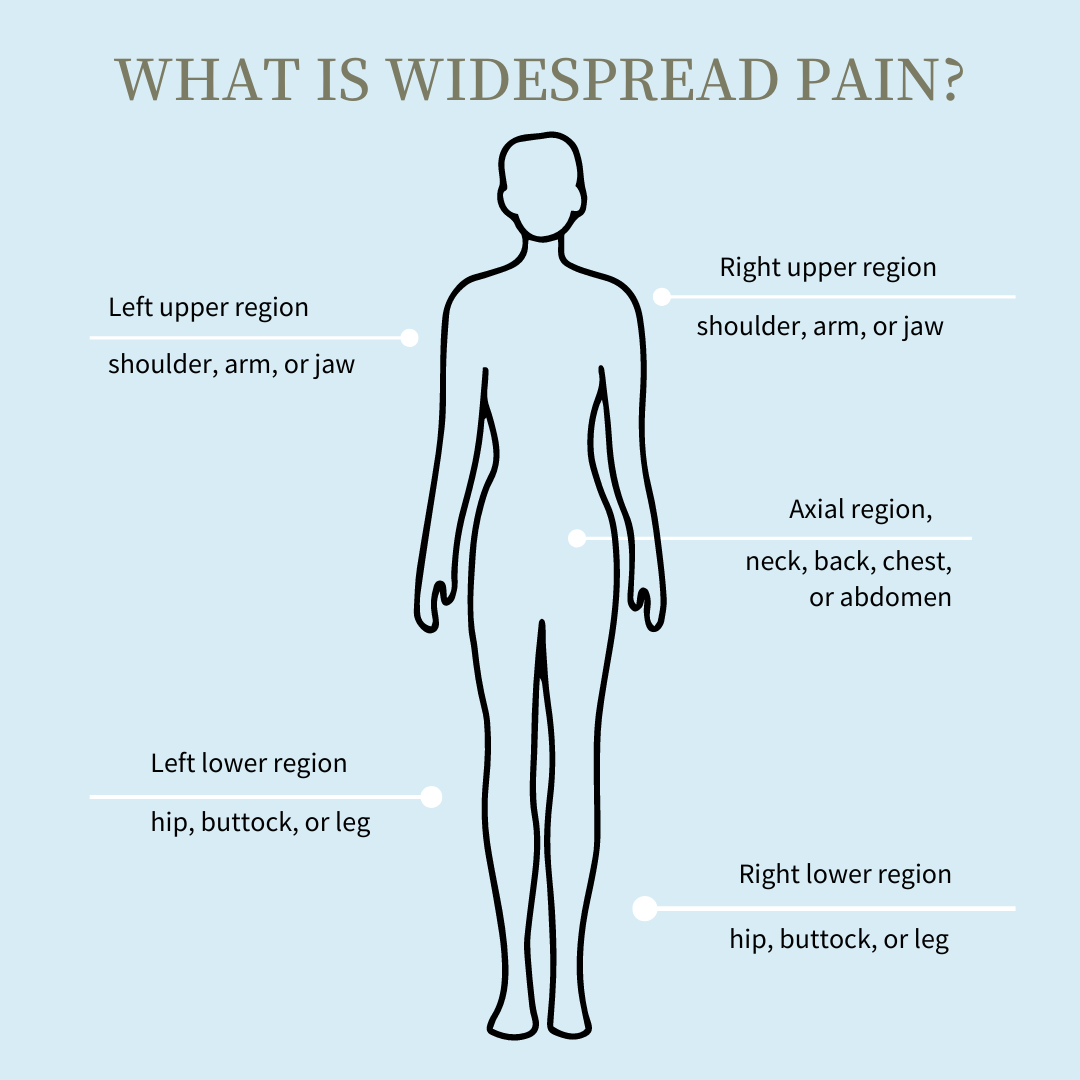
To be diagnosed with fibromyalgia, your pain must be present and consistent for at least three months, and the pain must affect at least four out of five body regions:
- left upper body
- right upper body
- left lower body
- right lower body
- lower back
If you meet these criteria, you may want to take a self-assessment for fibromyalgia. The Widespread Pain Index (WPI) and the Symptom Severity Scale (SSS) are two self-assessments for fibromyalgia developed in 2010 by the American College of Rheumatology (ACR). [5]
Widespread Pain Index
The Widespread Pain Index (WPI) lists 19 areas that may hurt when someone applies pressure to them. The WPI is a tool that helps you identify and report your pain points.
You must have at least 11 out of 19 positive pain points to be diagnosed with fibromyalgia. [3]
Symptom Severity Score
The Symptom Severity Score (SSS) helps you identify and evaluate symptoms that may indicate fibromyalgia.
The SSS has two parts:
Part SS2a evaluates
- The severity of your fatigue
- How often you awaken refreshed
- Your cognitive symptoms, such as memory or concentration problems
Part SS2b is a checklist of 41 symptoms associated with fibromyalgia. You score yourself based on the number of symptoms present.
- 0 symptoms = score of 0
- 1 to 10 symptoms = score of 1
- 11 to 24 = score of 2
- 25 or more = score of 3
Your total SSS is the sum of parts A and B.
You can use these self-assessments to determine if you could have fibromyalgia. If the test indicates you could, set up an appointment to talk to your doctor.
Your doctor may suspect fibromyalgia if you have a:
- WPI greater than or equal to 7 and a SS greater than or equal to 5 or
- WPI between 3 and 6 and an SS greater than or equal to 9.
Although the 2010 versions of the WPI and SSS are the fibromyalgia tests recommended by the American College of Rheumatology (ACR) and used by most doctors, researchers suggested modifications in 2016.
These modifications included adding a generalized pain requirement that looked at the presence of pain in four out of five areas of the body, as well as specifying that fibromyalgia can exist in the presence of other conditions as well as on its own.. [3]
The current method of defining and diagnosing fibromyalgia, even though it does not include a physical exam, like the previously-used tender point exam, correctly classifies nearly 90% of fibromyalgia cases, according to the American College of Rheumatology. [7] However, your doctor will likely want to learn more about your medical history and run further tests to rule out other conditions which might be causing your symptoms.
As part of this, your doctor may ask:
- Where is your pain located?
- How severe is your pain?
- How long have you had the pain?
- Do you have other symptoms?
- Do you have any other medical conditions?
Determining what is causing your pain and other symptoms is crucial to developing a proper treatment plan. [2] [7]
Lab Tests to Rule Out Other Conditions
Lab blood tests cannot diagnose fibromyalgia directly, but they can eliminate the possibility of other diagnoses with similar symptoms.
There are no objective markers in the blood for fibromyalgia, but blood tests can detect other conditions that may be causing your symptoms. Positive tests may indicate a different cause for your symptoms or may indicate you have another condition in addition to fibromyalgia. [5]
Thyroid Hormone Tests
Your doctor may recommend thyroid hormone tests. Thyroid blood tests measure the level of thyroid hormones in your system to determine how well your thyroid is functioning.
Low thyroid levels can cause symptoms similar to fibromyalgia, such as [5]
- Fatigue
- Weakness
- Muscle aches
- Memory problems
- Difficulty concentrating
Antibody tests
Your doctor may suggest antibody tests to determine if an autoimmune disease could be causing your symptoms. In an autoimmune disease, your body’s immune system attacks healthy tissue, causing inflammation.
Fibromyalgia is not an autoimmune disease, but some autoimmune diseases have similar or overlapping symptoms. [5]
ANA
An antinuclear antibody (ANA) test evaluates the antinuclear antibodies present in your blood.
Antinuclear antibodies are antibodies that attack healthy tissue in your body. ANAs in your blood could indicate you have an autoimmune disease.
Fibromyalgia is not associated with positive ANAs. [5]
ACCP
Anti-cyclic citrullinated peptide (CCP) antibodies indicate the possibility of rheumatoid arthritis, an autoimmune disease that shares symptoms with fibromyalgia. If you have a positive ACCP, your doctor may diagnose you with rheumatoid arthritis alone or in conjunction with fibromyalgia. [5]
Gluten Sensitivity
Your doctor may order a celiac serology to check for antibodies to gluten.
Celiac disease is an autoimmune disease in which your immune system reacts to gluten. Some symptoms of celiac disease are similar to fibromyalgia symptoms, such as:
- Abdominal pain
- Fatigue
- Joint aches
- Headaches
You may not be diagnosed with fibromyalgia if you have a positive gluten sensitivity, or you may be diagnosed with both. [5]
CRP
A C-reactive protein (CRP) test measures CRP levels in your blood.
High levels of CRP indicate inflammation and may be present in inflammatory forms of arthritis, such as rheumatoid arthritis. Since fibromyalgia is not an inflammatory disease, a positive CRP test may indicate you do not have fibromyalgia, or you have an inflammatory disease as well. [5]
ESR/Sed Rate
An erythrocyte sedimentation rate (ESR or sed rate) measures how quickly erythrocytes (red blood cells) separate from the other parts of the blood and settle to the bottom of the test tube as sediment. A high ESR or sed rate indicates inflammation in the body and suggests an inflammatory condition.
Since fibromyalgia is not an inflammatory disease, a high ESR may indicate you have another condition besides fibromyalgia. [5]
Tests without Support for Fibromyalgia
Blood Tests
Researchers and scientists are working to develop more specialized blood tests for fibromyalgia, but there is no currently accepted blood test to diagnose fibromyalgia, and more research is needed.
These blood tests check cytokine levels in your blood. Cytokines are chemical messengers in your blood that stimulate your immune system to attack a foreign substance. Low cytokine levels may indicate your body cannot fight infections or reduce inflammation as it should.
According to Rheumatology International, scientists are working on a specific blood test that may distinguish fibromyalgia from other inflammatory diseases, such as rheumatoid arthritis (RA), lupus erythematosus (SLE), or other inflammatory autoimmune conditions. [6] However, current tests cannot accurately differentiate between these conditions and fibromyalgia, and more research is needed.
Imaging Tests
Imaging tests like CTs, MRIs, or EEGs can test your muscles and brain for abnormalities. These tests can help researchers learn more about fibromyalgia, but they cannot detect the condition itself.
Like blood tests, imaging tests can diagnose or rule out other conditions, but they are not used to diagnose fibromyalgia. [5]
Performing a Fibromyalgia Self-Test
The American College of Rheumatology has proposed criteria to diagnose fibromyalgia: the Widespread Pain Index (WPI) and the Symptom Severity Scale (SSS). These tests are a self-assessment for fibromyalgia.
Swing Care has a free version of this fibromyalgia self-assessment test you can access here. Click “Take the Quiz” and follow the instructions.
If this test indicates you may have fibromyalgia, talk to your doctor. A self-test is an excellent way to start the diagnostic process, but a firm fibromyalgia diagnosis will require:
- A doctor’s assessment
- A medical chart review
- Blood and imaging tests to rule out other possible conditions
- A complete medical history, including your medical conditions, the medications and supplements you are taking, and your socioeconomic conditions
Your doctor will look at your fibromyalgia self-test along with these other factors and determine if you have fibromyalgia alone or in conjunction with other medical conditions.
Your doctor may refer you to a specialist, such as a rheumatologist or endocrinologist, if something other than fibromyalgia could be causing your symptoms.
These specialists can examine the complete medical picture and decide on your condition. They may determine you have fibromyalgia, a different medical condition, or a combination. [4]
Summary
Fibromyalgia can be complicated, and diagnosing the condition may be challenging.
Self-assessments are available to help you determine if fibromyalgia could be causing your symptoms. A fibromyalgia self-assessment, physical exams, and blood and imaging tests to rule out other conditions can help your doctor determine what is causing your symptoms and develop a plan of action.
If you have symptoms of fibromyalgia, take a self-assessment and talk to your doctor.
Medically reviewed by Dr. Andrea Chadwick, MD, MSc, FASA
Sources
- Behm, Frederick G., Igor M. Gavin, Oleksiy Karpenko, Valerie Lindgren, Sujata Gaitonde, Peter A. Gashkoff, and Bruce S. Gillis. “Unique Immunologic Patterns in Fibromyalgia.” BMC Clinical Pathology 12, no. 1 (December 17, 2012): 25. https://doi.org/10.1186/1472-6890-12-25.
- Branch NSC and O. Fibromyalgia. National Institute of Arthritis and Musculoskeletal and Skin Diseases.
- Galvez-Sánchez, Carmen M., and Gustavo A. Reyes del Paso. “Diagnostic Criteria for Fibromyalgia: Critical Review and Future Perspectives.” Journal of Clinical Medicine 9, no. 4 (April 23, 2020): 1219. https://doi.org/10.3390/jcm9041219.
- Häuser, Winfried, and Mary-Ann Fitzcharles. “Facts and Myths Pertaining to Fibromyalgia.” Dialogues in Clinical Neuroscience 20, no. 1 (March 31, 2018): 53–62. https://doi.org/10.31887/DCNS.2018.20.1/whauser.
- Testing for fibromyalgia | arthritis foundation.
- Wallace, Daniel J., Igor M. Gavin, Oleksly Karpenko, Farnaz Barkhordar, and Bruce S. Gillis. “Cytokine and Chemokine Profiles in Fibromyalgia, Rheumatoid Arthritis and Systemic Lupus Erythematosus: A Potentially Useful Tool in Differential Diagnosis.” Rheumatology International 35, no. 6 (June 1, 2015): 991–96. https://doi.org/10.1007/s00296-014-3172-2.
- Wolfe F, et al. (2010). The American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and Measurement of Symptom Severity.
