Chronic pain is often viewed as the hallmark symptom of fibromyalgia. However, there are many more symptoms associated with fibromyalgia, which can leave you questioning whether your symptoms are related to fibromyalgia, or another condition.
In this article, explore the list of fibromyalgia symptoms and learn more about what causes these symptoms, such as joint pain all over the body, aching bones and muscles, & tiredness. Read on for signs of fibromyalgia, both common and rare fibromyalgia symptoms, and take your own fibromyalgia symptoms quiz.
First Symptoms of Fibromyalgia
So, what are usually the first signs of fibromyalgia? Because there are a variety of signs and symptoms associated with fibromyalgia, it can be confusing to know if the symptoms you are experiencing are related to fibromyalgia or not. To help with this, we’ve broken the symptoms of fibromyalgia down into the first commonly noticed signs, followed by fibromyalgia flare-ups and the symptoms that can come with these flares. Lastly, we’ll take a look at the rare symptoms of fibromyalgia.
Chronic Whole Body Pain
The trademark symptom of fibromyalgia is widespread or whole-body pain. This involves pain in multiple areas, such as upper neck pain, back pain, arms and leg pain – however, the pain can migrate throughout the body to any different region. In fact, in 2016 the diagnostic criteria for fibromyalgia was updated to require pain in four out of five areas of the body, replacing the prior tender-point exam.
Why do people with fibromyalgia experience widespread pain? Current research suggests that the way in which pain is processed in the central nervous system (CNS) is amplified in someone with fibromyalgia. This process, called central sensitization, is thought to play a key role in developing chronic pain within fibromyalgia. Central sensitization involves the entire CNS becoming hypersensitive to pain, which can result in pain feeling more severe and lasting for a longer period.1
Brain studies2 support the role of central sensitization in chronic whole-body pain, as they have highlighted increased connectivity in systems that amplify pain signals and decreased connectivity in systems that reduce the processing of pain.
The pain in fibromyalgia is often felt throughout your body, but can be worse in particular areas such as your neck or back. For the pain to be chronic, it must last for at least three months, although it may get better or worse at different times. For the pain to be classified as ‘whole body,’ pain must be felt in at least four out of the five areas below:
- Right upper region (shoulder, arm)
- Left upper region (shoulder, arm)
- Axial region (neck, back)
- Left lower region (left hip, leg)
- Right lower region (right hip, leg).
If you feel pain in these areas, it does not necessarily mean you have fibromyalgia. It is always best to speak to a doctor about your symptoms, so they may rule out other causes of the pain.
Fatigue and Sleeplessness
Another common symptom of fibromyalgia is fatigue and sleeplessness. This can range from feeling mild fatigue to exhaustion, which can often leave you feeling unrefreshed or listless. A review of multiple studies within this area consistently found a link between fibromyalgia and fatigue, with 76% of people with fibromyalgia reporting fatigue.3
This study also identified terms in which people with fibromyalgia described their fatigue, which may help you identify the fatigue you may experience. These included:
- “An inescapable or overwhelming feeling of profound physical tiredness”
- “An uncontrollable, unpredictable constant state of never being rested”
- “Not relieved by rest”
- “Ghastly sensation of being totally drained of every fiber of energy”
Research has also found a common link between fibromyalgia and sleeplessness. A study that reviewed 16 other research studies found that reduced sleep quality, duration, efficiency and increased sleep disturbance were all present in individuals with fibromyalgia.4 Another study found 576 out of 600 people with fibromyalgia reported problems with sleep.5 These difficulties with sleep also predicted the amount of pain people felt, indicating a link between fibromyalgia, reduced sleep and pain.
Cognitive Symptoms
Cognitive symptoms, which are also termed brain fog or “fibro fog,” include a variety of symptoms such as:
- Having trouble remembering things
- Problems with attention and concentration
- Inhibited verbal skills such as slow speech
- Finding it difficult to think clearly
These cognitive symptoms can greatly impact your everyday life and are seen as primary symptoms.6 Evidence for fibro fog has come from a variety of studies6; one review of 37 studies compared individuals with fibromyalgia with people without fibromyalgia on a variety of neuropsychological measures.7 They found individuals with fibromyalgia to have poorer performance in their short- and long-term memory, the speed at which information is processed, and other cognitive domains.
One theory for these cognitive symptoms is based on the interference effects of pain. Studies show that when pain increases, cognitive decline increases.6 This could be because pain is an attention-demanding stimulus which uses brain areas that are also used in cognitive abilities such as memory. So, if your attention is directed more to your pain, the less cognitive ability you may have to spare.
Based on research, chronic whole-body pain, fatigue, sleeplessness and cognitive symptoms tend to be the first signs and symptoms of fibromyalgia. Now, let’s take a look at fibromyalgia flare symptoms.
Fibromyalgia Flare Symptoms
Fibromyalgia symptoms occur on a spectrum and can vary in intensity from day-to-day or even month-to-month. This can result in fibromyalgia flare-ups, where pain is particularly intense. There can be a variety of triggers of fibro flare ups such as poor sleep, stress, overexertion, anxiety, certain foods and more. Let’s dive into some of the fibromyalgia flare-up symptoms.
Increased Pain
We know that whole-body pain is one of the dominant symptoms of fibromyalgia, but this pain can increase and decrease over time. Due to this varying nature of pain, it is not surprising that when a fibro flare up occurs, an increase in pain can often be the first symptom.
Imagine a volume control knob on a radio; when turned up, the volume increases and vice versa. This is like what happens when you have a fibromyalgia flare-up. Because of a trigger, that volume knob turns up high, resulting in heightened pain, which also can increase other symptoms too such as fatigue and fibro fog.
Muscle Aches
As fibromyalgia causes pain throughout the musculoskeletal system, it’s common for muscle aches to occur. Again, central sensitization plays a key role in muscle aches. Also, myofascial trigger points, which are localized tight spots in the muscles, are related to muscle aches and spasms in fibromyalgia. However, this link is inconclusive.
Muscle aches tend to be described as dull and achy, but it can also feel as if your muscles have been ‘pulled’ or overworked, even though you have not exercised. The muscle aches you experience can also feel like having knots in the muscle or general tightness.
Muscle aches can also be accompanied by spasms or twitches. Spasms are when the muscle contracts continuously and uncontrollably. On the other hand, twitching is when a nerve signal is sent to a muscle, resulting in the muscle contracting uncontrollably and very briefly, as if it jumps. In summary, muscle aches are common in fibromyalgia and can manifest in different ways.
Joint Stiffness, Numbness and tingling
Fibro flare ups can be accompanied by joint stiffness, particularly if you have been sitting in the same position for long.8 This stiffness can occur within multiple areas. Numbness and tingling can also occur in fibromyalgia, often in the arms, hands, legs and feet. This can raise concern about other difficulties involving nerves (e.g, carpal tunnel syndrome); so one should always consult your doctor if you are unsure or worried about what might be causing numbness and tingling or stiffness.
Migraines or IBS
Migraines are intense headaches accompanied with a throbbing pain, typically on one side of the head. Research has found that individuals with fibromyalgia are likely to experience migraines9; a large scale survey study found 55.8% of people with fibromyalgia reported experiencing migraines as well as their fibromyalgia symptoms.10 As migraines are also related to experiencing pain, central sensitization is again thought to be involved in the link between fibromyalgia and migraines. Due to this, research has also found that migraines experienced in fibromyalgia are more frequent, intense and severe.11
On the other hand, irritable bowel syndrome (IBS) is a digestive condition which can result in bloating in your stomach, pain, constipation or diarrhea. Some research suggests that nearly 70% of people with fibromyalgia experience IBS symptoms, with pain being a primary symptom of both.12 It is not understood why they both can occur together so frequently, however, the processing of pain in the brain is again a potential reason for this.
Rare Symptoms of Fibromyalgia
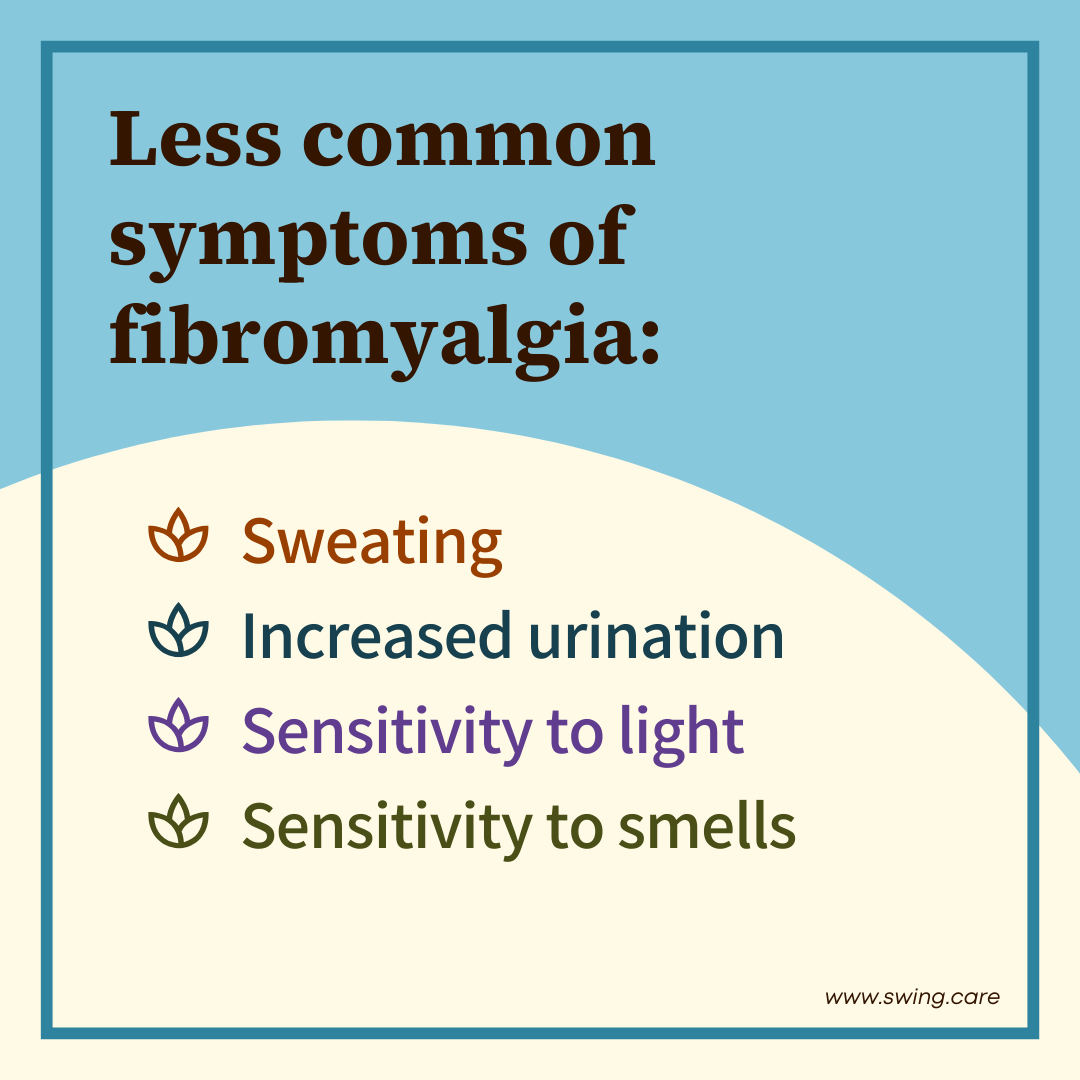
So we’ve taken a look at the most common symptoms of fibromyalgia and also symptoms of fibromyalgia flare-ups. Let’s dive into the rare symptoms that are less commonly experienced.
Sensory Sensitivity
Sensory sensitivity refers to our bodies reacting very strongly to different stimuli such as noise, bright or flashing lights, smells, tastes and more. Studies have increasingly linked fibromyalgia and sensory sensitivity. One study conducted fMRIs on women with fibromyalgia to examine the brain’s response to different sensory stimuli.13 They found individuals with fibromyalgia reported an increased subjective sensitivity to stimuli and their brain responses to these stimuli were weakened. This weakened brain response was correlated to subjective hypersensitivity, indicating sensory sensitivity may be a symptom of fibromyalgia.
It’s still unclear why there is a link between fibromyalgia and sensory sensitivity, but it is thought this is due to the brain’s change in processing pain; the hypersensitive CNS in fibromyalgia patients may result in the nervous system reacting more to various other stimuli.14
Increased Sweating or Urination
Another rare symptom of fibromyalgia is increased sweating or urination. There is less research on these symptoms, but increased sweating is thought to occur due to autonomic nervous system dysfunction15, which can alter physiological responses within the body. Also, hypersensitivity (as described above) to heat can contribute to increased sweating.
Research has also linked an overactive bladder with fibromyalgia, with one recent study finding that 93% of patients with fibromyalgia reported an overactive bladder.16 However, their sample size was only 27 patients, limiting these findings. However, it can be important to know that this can be a symptom of fibromyalgia (albeit rare). If you do experience it, you can always speak to your doctor to see what may help.
Take the Fibromyalgia Self-Assessment
As there are a lot of symptoms of fibromyalgia, symptoms and their severity will always vary from person to person. Someone may experience more severe chronic pain, fatigue and IBS, while another person may experience pain with cognitive symptoms and numbness.Because of the variety of symptoms, it can be helpful to take your own fibromyalgia self-assessment. You can take the fibromyalgia quiz here to go through the diagnostic criteria on your own and get your score.
With the right diagnosis and treatment, you can look forward to fewer pain days and more freedom to do the things that matter most to you.
Medically reviewed by Dr. Andrea Chadwick, MD, MSc, FASA
Sources
1. Nijs J, George SZ, Clauw DJ, Fernandez-De-Las-Penas C, Kosek E, Ickmans K, Fernandez-Carnero J, Polli A, Kapreli E, Huysmans E, Cuesta-Vargas AI, Mani R, Lundberg M, Leysen L, Rice D, Sterling M, Curatolo M. Central sensitization in chronic pain conditions: Latest discoveries and their potential for precision medicine. Lancet Rheumatol. 2021 May;3(5):E383-E392. doi:10.1016/S2665-9913(21)00032-1
2. Cagnie B, Coppieters I, Denecker S, Six J, Danneels L, Meeus M. Central sensitization in fibromyalgia? A systematic review on structural and functional brain MRI. Semin Arthritis Rheum. 2014 Aug;44(1):68-75. doi: 10.1016/j.semarthrit.2014.01.001. Epub 2014 Jan 8. PMID: 24508406.
3. Vincent A, Benzo RP, Whipple MO, McAllister SJ, Erwin PJ, Saligan LN. Beyond pain in fibromyalgia: insights into the symptom of fatigue. Arthritis Res Ther. 2013;15(6):221. doi: 10.1186/ar4395. PMID: 24289848; PMCID: PMC3978642.
4. Keskindag B, Karaaziz M. The association between pain and sleep in fibromyalgia. Saudi Med J. 2017 May;38(5):465-475. doi: 10.15537/smj.2017.5.17864. PMID: 28439595; PMCID: PMC5447206.
5. Bigatti SM, Hernandez AM, Cronan TA, Rand KL. Sleep disturbances in fibromyalgia syndrome: relationship to pain and depression. Arthritis Rheum. 2008 Jul 15;59(7):961-7. doi: 10.1002/art.23828. PMID: 18576297; PMCID: PMC3691959.
6. Galvez-Sánchez CM, Reyes Del Paso GA, Duschek S. Cognitive Impairments in Fibromyalgia Syndrome: Associations With Positive and Negative Affect, Alexithymia, Pain Catastrophizing and Self-Esteem. Front Psychol. 2018 Mar 22;9:377. doi: 10.3389/fpsyg.2018.00377. PMID: 29623059; PMCID: PMC5874325.
7. Bell T, Trost Z, Buelow MT, Clay O, Younger J, Moore D, Crowe M. Meta-analysis of cognitive performance in fibromyalgia. J Clin Exp Neuropsychol. 2018 Sep;40(7):698-714. doi: 10.1080/13803395.2017.1422699. Epub 2018 Feb 1. PMID: 29388512; PMCID: PMC6151134.
8. Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, Fitzcharles MA, Paiva ES, Staud R, Sarzi-Puttini P, Buskila D, Macfarlane GJ. AAPT Diagnostic Criteria for Fibromyalgia. J Pain. 2019 Jun;20(6):611-628. doi: 10.1016/j.jpain.2018.10.008. Epub 2018 Nov 16. PMID: 30453109.
9. Penn IW, Chuang E, Chuang TY, Lin CL, Kao CH. Bidirectional association between migraine and fibromyalgia: retrospective cohort analyses of two populations. BMJ Open. 2019 Apr 8;9(4):e026581. doi: 10.1136/bmjopen-2018-026581. PMID: 30962236; PMCID: PMC6500182.
10. Vij B, Whipple MO, Tepper SJ, Mohabbat AB, Stillman M, Vincent A. Frequency of Migraine Headaches in Patients With Fibromyalgia. Headache. 2015 Jun;55(6):860-5. doi: 10.1111/head.12590. Epub 2015 May 21. PMID: 25994041.
11. Whealy M, Nanda S, Vincent A, Mandrekar J, Cutrer FM. Fibromyalgia in migraine: a retrospective cohort study. J Headache Pain. 2018 Jul 31;19(1):61. doi: 10.1186/s10194-018-0892-9. PMID: 30066109; PMCID: PMC6068065.
12. Chang L. The association of irritable bowel syndrome and fibromyalgia. Unc Center For Functional GI & Motility Disorders [Internet]. 2017 [cited 2023 Jul 18]; Available from: https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/Fibromyalgia-and-IBS.pdf
13. López-Solà M, Pujol J, Wager TD, Garcia-Fontanals A, Blanco-Hinojo L, Garcia-Blanco S, Poca-Dias V, Harrison BJ, Contreras-Rodríguez O, Monfort J, Garcia-Fructuoso F, Deus J. Altered functional magnetic resonance imaging responses to nonpainful sensory stimulation in fibromyalgia patients. Arthritis Rheumatol. 2014 Nov;66(11):3200-9. doi: 10.1002/art.38781. PMID: 25220783; PMCID: PMC4410766.
