If you’re living with fibromyalgia, you’re probably already well aware that pain is its main symptom. Fibromyalgia can cause pain symptoms throughout the entire body and musculoskeletal system that can vary from person-to-person. But there are many possible causes of pain. How do you know if you have fibromyalgia?
To diagnose fibromyalgia, doctors check in several different fibromyalgia pain areas of your body using an assessment called the Widespread Pain Index (WPI). They’ll also ask you about issues like fatigue and sleep problems. In this article, we’ll discuss the different fibromyalgia pain areas in the WPI. We’ll talk about other fibromyalgia symptoms besides pain. And finally, we’ll cover the basics of treating fibromyalgia pain.
With the right diagnosis and treatment, you can look forward to fewer pain days and more freedom to do the things that matter most to you.
What Is the Widespread Pain Index?
Many common health conditions can be diagnosed using a lab test or scan. For example, arthritis causes changes in the joints that are usually visible on an MRI or x-ray. High cholesterol is a serious problem, but it has no symptoms. It can be diagnosed only through blood tests. Fibromyalgia is different. There is no lab test or imaging scan that reveals that a person has it.
In the past, doctors diagnosed fibromyalgia by checking for what were called “tender points.” There were 18 points designated on the body. In a diagnostic exam, the doctor would press on these spots to test for pain. If a person had pain in 11 or more of the 18 spots, they were considered to have fibromyalgia.
In 2016, the American College of rheumatology developed a new set of criteria for diagnosing fibromyalgia.¹ Now, a person is diagnosed with fibromyalgia when they have
- “significant and widespread pain,”
- severe symptoms (like fatigue), and
- the pain and other symptoms have been “generally present” at least three months.
Everyone experiences pain a little differently. What counts as “significant and widespread pain”?
To make this determination, doctors use an assessment called the Widespread Pain Index, or WPI. The WPI is a questionnaire that asks whether you have experienced pain in a certain region of your body in the past week. Your doctor considers your answers to these questions about pain alongside other symptoms to determine whether fibromyalgia is the best explanation for what you’re experiencing.
Fibromyalgia pain is most often described as a dull and constant achy feeling, as opposed to intermittent, sharp pain (although people with fibromyalgia often experience pain flares, or periods of heightened pain severity). It is typically experienced as muscle pain, though it may also show up as joint pain. And the pain tends to occur on both sides of the body,and in both the upper and the lower body.
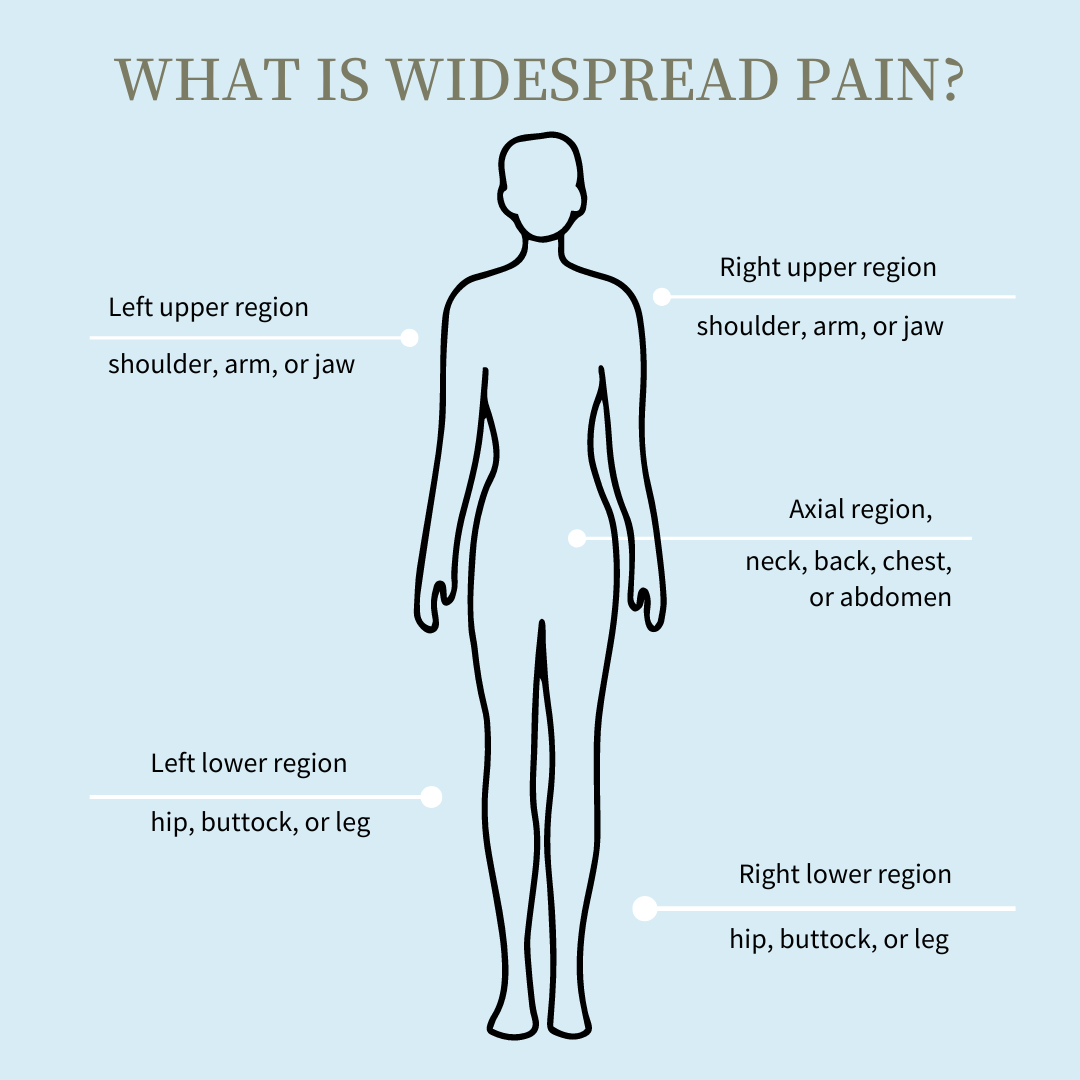
To assess for fibromyalgia pain, the WPI asks about pain in five general regions of the body: above the waist on the left, above the waist on the right, below the waist on the left, below the waist on the right, and central. Let’s take a closer look at these fibromyalgia pain areas.
Shoulder
The first two questions are about whether you have had pain in the shoulder girdle on the right or left side. “Shoulder girdle” refers to the area from the base of the neck to the shoulder point, and extending slightly forward and back. Picture a saddle resting on each shoulder.
Arm
Continuing with the upper right and left quadrants of the body, the WPI asks about pain in the upper arm, between the shoulder and elbow, and in the lower arm, between elbow and wrist.
Hip
Moving to the lower right and left sides of the body, the next questions on the WPI are whether you’ve experienced pain in either hip or buttock.
Leg
Continuing with the lower body, the WPI asks whether you’ve experienced pain in the upper left leg, upper right leg, lower left leg, or lower right leg.
Jaw
Moving to the axial (central) region of the body, the next two questions are whether you’ve experienced pain in your jaw, on the right or left side.
Chest
Continuing with the axial region, the WPI asks whether you have had pain in your chest.
Abdomen
The WPI asks next whether you’ve experienced abdominal pain.
Neck
Continuing with the axial region, the WPI asks about pain in the front or back of the neck.
Back
Finally, the WPI asks whether you’ve had pain in your upper back or lower back.
Other Diagnostic Criteria for Fibromyalgia
While significant widespread pain is the hallmark of fibromyalgia, it is not the only symptom. A person is diagnosed with fibromyalgia when they have certain other symptoms in addition to the pain. These include things like fatigue, sleep problems, and brain fog or trouble thinking clearly.
Introduction to the Symptom Severity Scale
To evaluate these other fibromyalgia symptoms, doctors use an assessment called the Symptom Severity Scale (SSS) along with the Widespread Pain Index. The first part of the SSS focuses on the three symptom areas that are characteristic of fibromyalgia. It asks how severe and bothersome each of these has been over the past week.
Cognitive Symptoms
Many people with fibromyalgia experience changes in their thinking and memory. It can be difficult to focus, concentrate, or pay attention. It can also be hard to remember things that happened recently. Some people refer to this experience as “fibro fog.”
Fatigue
Fibromyalgia can leave you with a feeling of tiredness that doesn’t go away no matter how much you sleep. Fatigue can be felt at any time of day – morning, afternoon, or evening. Fibromyalgia can drain your energy to the point that normal everyday activities seem overwhelming.
Waking Unrefreshed
When you have fibromyalgia, you may wake up feeling tired even when you’ve gotten several hours of sleep. In addition, many people with fibromyalgia experience insomnia or other sleep disturbances, such as waking often during the night or sleeping very lightly in the early morning hours. This can make it difficult to get enough sleep, and it adds to the feeling of exhaustion.
Other Somatic Symptoms
Fibromyalgia can involve a number of other somatic (body) symptoms. The second part of the Symptom Severity Scale asks whether you’ve had these experiences in the past seven days. The additional symptoms include things like headache, depression, nervousness, nausea, diarrhea, shortness of breath, and bladder issues.
Why Tender Points Are No Longer Used to Assess Fibromyalgia Pain Areas
Together, the Widespread Pain Index and the Symptom Severity Scale give a complete picture of whether you are experiencing symptoms that are best described as fibromyalgia. In making a diagnosis, your doctor will consider how severe your symptoms are, how long they have lasted, and what other medical conditions might be playing a role. You can also take a fibromyalgia quiz that’s self-guided to go through the criteria; although it is not an official diagnosis, it can help you begin that conversation with your provider.
Since there is no lab test or scan that shows whether a person has fibromyalgia, the condition has always been diagnosed through more subjective assessments like a medical history and physical exam. However, the protocol for making a diagnosis has been refined and improved in recent years to be more accurate.
If you’ve had fibromyalgia symptoms for a while, you may have heard of tender points. You may even originally have been diagnosed using this kind of exam. If that’s the case, you may be wondering why tender points are no longer used to assess fibromyalgia pain.
Researchers noticed a number of problems with diagnosing fibromyalgia mainly based on the tender point exam. Many doctors did not know how to examine tender points or did the tender point exam incorrectly. In addition, the tender point exam did not take into account the other symptoms – fatigue, cognitive issues, and waking unrefreshed – that are now understood to be central to fibromyalgia. For these reasons, the American College of Rheumatology updated its criteria in 2011 to recommend diagnosing fibromyalgia based on the Widespread Pain Index plus the Symptom Severity Scale.²
Treating Fibromyalgia Pain
Getting an accurate diagnosis is the first step in getting help. Once your doctor has confirmed that fibromyalgia is the cause of your symptoms, you can start exploring which treatments will work best for you.
Keeping a Pain Diary
To get a better picture of your experience of fibromyalgia, you may find it helpful to keep a record of your symptoms. When do you have pain? How strong is it? What makes it better, and what makes it worse? Note your other symptoms, too, like fatigue and brain fog. Write down how you sleep each night and how you feel when you wake in the morning. This record of your pain and other symptoms can give you a sense of your baseline. It can also help you and your doctor decide where to start in treating your fibromyalgia.
Discussing Medication with Your Doctor
Medications are commonly used to help with fibromyalgia symptoms. For pain, your doctor may recommend over-the-counter meds such as acetaminophen (Tylenol) or ibuprofen (Advil). Opioid medications are not used as pain meds for fibromyalgia. They have major side effects and can actually make your pain worse. Certain antidepressants can help with pain, fatigue, and sleep issues. Anti-seizure drugs such as gabapentin (Neurontin) and pregabalin (Lyrica) can help manage fibromyalgia pain. Talk with your doctor about whether medications could be helpful for your symptoms.
Non-Drug Treatment Options
Medication is not the only treatment for fibromyalgia pain. There are a number of other things that can help. In fact, some people with fibromyalgia find that non-drug treatments work better than medications.
Cognitive behavioral therapy (CBT) can be very effective as a treatment for fibromyalgia pain. CBT and related therapies such as acceptance and commitment therapy (ACT) help you work with your thoughts and behaviors. Many people who live with pain find that worrying that the pain will never go away, or that it will get worse, or that the pain means something harmful is happening to their body, can make their symptoms worse. By practicing CBT strategies, you can learn to see your symptoms differently. As a result, you may experience much less suffering and more freedom to do the things that are most important to you.
Stress and anxiety can also worsen pain and other symptoms, so relaxation and stress-reduction techniques can be helpful in managing fibromyalgia. You might try mindfulness meditation, guided visualization, or breathing techniques. These help you shift into a more peaceful, relaxed state of being.
The achiness, soreness, and stiffness associated with fibromyalgia can make you want to hold still. Many people with fibromyalgia worry that physical activity will make their pain flare up. And, if you overdo it, this could happen. But when you take a gentle pace and work up to it gradually, exercise can be very beneficial in reducing fibromyalgia pain. A physical therapist can help you design a program of stretching, strengthening, and movement that is just right for your body. The same principle of pacing yourself can also be helpful in regular daily activities like household chores and errands.
Good treatment for fibromyalgia reduces your suffering as well as your pain. Your doctor is likely to start with an assessment using the Widespread Pain Index and Symptom Severity Scale. And, depending on the results, medication may be recommended. However, for best results, you’ll want to consider non-drug treatments too.
Learn more about the self-report survey, how fibromyalgia diagnosis has changed over time, and how you can work with a provider or a Swing Care physician toward a diagnosis.
Medically Reviewed by Dr. Andrea Chadwick, MD
Sources
¹ Wolfe, F., Clauw, D. J., FitzCharles, M., Goldenerberg, D., Häuser, W., Katz, R. S., Russell, I. J., Mease, P. J., Russell, A., & Walitt, B. (2016). 2016 Revisions to the 2010/2011 Fibromyalgia Diagnostic Criteria [abstract]. Arthritis Rheumatol. 68 (suppl 10). https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/
² Wolfe, F., Clauw, D. J., FitzCharles, M., Goldenerberg, D., Häuser, W., Katz, R. S., Russell, I. J., Mease, P. J., Russell, A., & Walitt, B. (2016). 2016 Revisions to the 2010/2011 Fibromyalgia Diagnostic Criteria [abstract]. Arthritis Rheumatol. 68 (suppl 10). https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/












